What Are Standard Precautions? Infection Control Facility Guide

Safety in healthcare is a big issue. Workers’ compensation claims show that hospital employees sustain more incidences of illness than workers in other high risk industries. On any given day, 1 in 31 hospital patients suffer from a hospital-acquired infection. Failure to follow standard precautions is often the culprit. But what are standard precautions?
Standard precautions in healthcare are infection control protocols that help prevent healthcare-acquired infections and protect frontline staff delivering care. Yet, healthcare leaders must provide staff with adequate education, training, and resources for those protective environmental precautions to be effective.
Terminology for infection control protocols may vary by region. For example, healthcare professionals in the U.K. apply the 10 principles of infection control. We’ll provide a helpful breakdown of the Centers for Disease Control and Prevention (CDC) standard precautions that are used in the U.S. We’ll also cover the rationale for each category and share tips for how to better incorporate them into your organizational practices and policies to promote safety and support compliance efforts.
What Is Infection Control?
Before we answer the question, What are standard precautions? it’s important to learn the basics of infection control. Generally, these are policies and procedures meant to prevent and reduce infection rates.
Hospitals in the U.S. began implementing infection control policies in the 1950s after recognizing the occurrence of healthcare-associated infections (HAIs). Examples include central line-associated bloodstream infections (CLABSIs) or catheter-associated urinary tract infections (CAUTIs). Occupational acquired infections can happen through contaminated needlestick injuries, or exposure to blood-borne pathogens.
Healthcare organizations can create a culture of safety by incorporating an infection control department dedicated to preventing and reducing infections. Infection control committees are responsible for conducting surveillance of infection rates and preventing the spread of infectious agents through clinical policies and practice guidelines.
However, your organization doesn’t need to create infection-prevention strategies from scratch. Resources from the Healthcare Infection Control Practices Advisory Committee (HICPAC) are available to guide revamping initiatives around protective environmental precautions. The same committee also provides advice for infection control policies to federal organizations like the CDC and HHS about the prevention, surveillance, and control of HAIs across healthcare settings, from hospitals to home health.
What Are Standard Precautions for Infection Control?
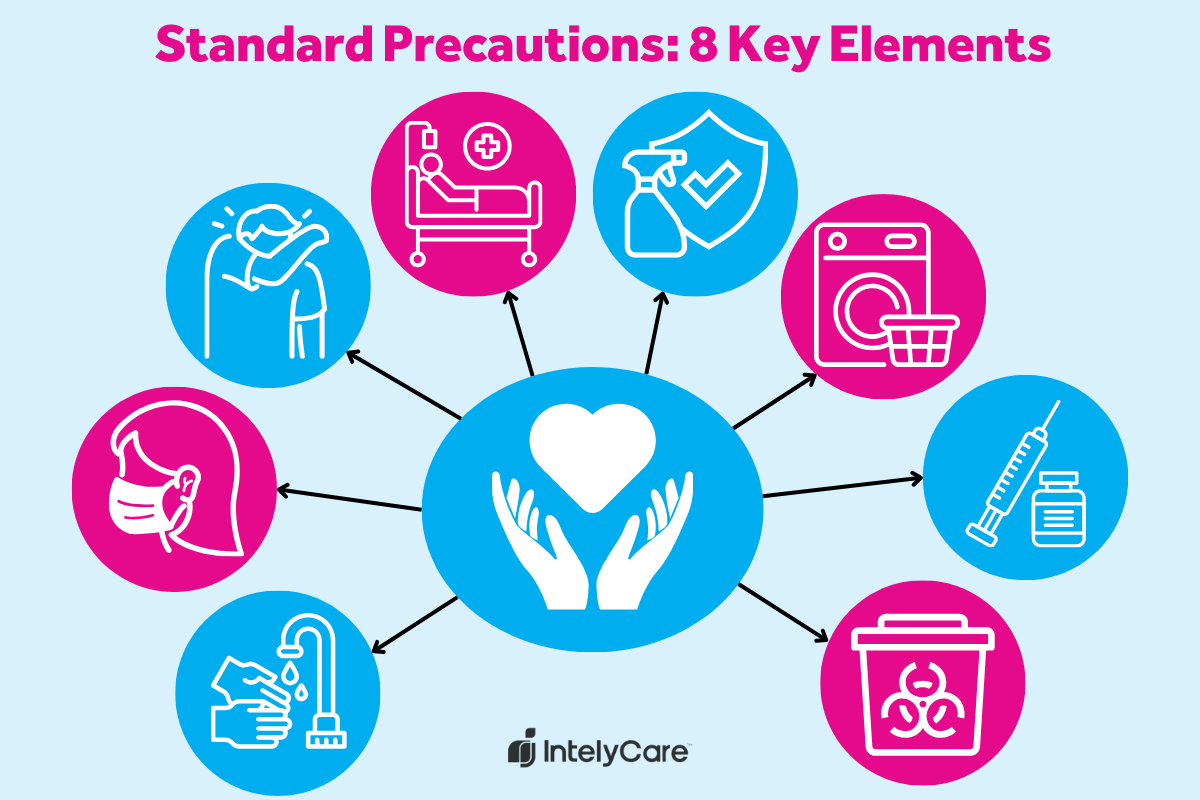
Healthcare staff must assume every interaction in the practice setting — whether with patients, visitors, or other staff — carries a risk of infectious exposure. This practice, known as standard precautions, should be used during all instances of clinical care. Within the guidelines, there are eight elements that establish the minimum requirements for maintaining standard precautions in healthcare. Some of these standard precautions include:
- Performing hand hygiene.
- Handling laundry and textiles with care.
- Following safe injection practices.
When caring for a patient with a recognized infection, healthcare staff follow transmission-based precautions in addition to standard precaution measures. These are categorized by route of transmission, as outlined in the table below.
| Transmission-Based Precautions | |
|---|---|
| Contact Precautions | Used for patients with a known or suspected infection that can be spread by touch, such as methicillin-resistant Staphylococcus aureus (MRSA) |
| Droplet Precautions | Followed when germs may be spread through coughing or sneezing, such as influenza |
| Airborne Precautions | Used for pathogens that are spread via the airborne route, such as measles or chickenpox |
What Are Standard Precautions vs. Universal Precautions?
You’ve probably heard both terms and are now wondering which is correct. Is it standard precautions or universal precautions? Universal precautions was the predecessor to standard precautions in healthcare and targeted prevention of infection from bloodborne pathogen exposure, such as HIV and Hepatitis B during patient care. The key difference is that the standard precaution approach applies to all patients and potential sources of infection, whereas universal precautions focus almost exclusively on blood-borne pathogens.
8 Key Elements of Standard Precautions in Healthcare
What are the CDC’s standard precautions recommendations designed to do? They serve as guidelines to help drive clinical decisions in the healthcare setting. When establishing policies for staff, it’s important to consider organizational policies, CMS regulations, and other occupational safety standards that weigh into practice guidelines and determine compliance.
Below are the essential components of infection control according to the CDC standard precautions.
1. Perform Hand Hygiene
Handwashing is one of the most effective ways to prevent the spread of infection in the healthcare setting. Staff training on proper handwashing should include information about:
- When to use soap and water vs. alcohol-based sanitizer.
- Frequency and duration of handwashing.
- Handwashing before sterile procedures.
Tip: Make your training course about hand hygiene interactive with an ultraviolet light demonstration to visualize germs and assess handwashing effectiveness.
2. Wear Personal Protective Equipment (PPE)
Any time there’s an expectation of possible transmission of infection, staff should don appropriate PPE. Facility policies should also direct staff to place patients on isolation precautions based on the type of infection suspected or recognized.
Tip: Consider environmental barriers to donning the proper PPE, and redesign spaces to make accessing standard precautions easier. For example, implement isolation PPE carts to avoid supplies being tucked into handrails or forgotten in the midst of other patient care requirements.
3. Practice Respiratory Hygiene
Practicing respiratory etiquette when coughing or sneezing prevents the spread of infection through droplets. Facilities can post educational reminders to “cover your cough” and provide visual demonstrations of sneezing etiquette. Place alcohol-based sanitizer throughout public spaces to encourage hand hygiene when coughing or sneezing.
Tip: For patients on droplet precautions, offer a variety of masks (such as two different colors to choose from) to promote adherence and autonomy during instances of required wear, like during transport through the halls.
4. Patient Placement
When deciding where a patient is placed within a facility or unit, decision-makers must take into account any infection risks. For example, a patient with a recognized infection should be placed in a single room instead of a shared room. Facility-based policies regarding patient placement should reinforce the CDC’s guidelines for isolation precautions.
Tip: Coordinate a standard of practice in patient transfers that establishes a stop-gap around communicating isolation status. This can prevent accidentally assigning a patient with known infectious risk factors to a double room or the provision of clinical care without the proper healthcare precautions.
5. Clean and Disinfect Equipment and Environment
What are standard precautions that pertain to the environment? For starters, maintaining a clean environment is the responsibility of all healthcare staff, not just environmental services staff. Policy guides should inform staff which equipment is classified as single-use, single-patient use, or reusable. Staff can do their part to maintain a clean environment by:
- Disinfecting high-touch surfaces in patient rooms and shared workspaces.
- Cleaning reusable equipment between patients.
- Sending equipment to the sterile processing department as appropriate.
Tip: Utilize visual cues like signs outside of patient doors to indicate the type of clean necessary for room turnover. These indicators serve as communication fail-safes regarding the specific depth of cleaning necessary, while also keeping environmental staff safe.
6. Handle Textiles and Laundry Properly
Another way to protect patients is to prevent the spread of infection through bed sheets and patient gowns. Clean linens must be stored in a clean, designated place. Dirty linen should be discarded in a designated area. Facility policies should indicate the process of laundering linens exposed to infectious pathogens.
Tip: Consider partnering the infection control committee with an injury-prevention committee to conduct education and training on the importance of not overfilling patient laundry hampers and soiled textile bins. Overfull laundry undermines infection-control measures and risks staff injuries.
7. Follow Safe Injection Practices
Practicing needle safety protects patients from exposure to germs during an injection and protects staff from exposure to blood and bodily fluids. Healthcare leaders should create policies that guide staff in preventing unsafe injection practices, including:
- Never reusing an insulin pen on more than one person.
- Wearing a mask during lumbar punctures (spinal taps).
- Never reusing a fingerstick device on more than one person.
Tip: Require attendance at demonstrations or training for any new product that features a sharps device. If a team member cannot attend one of the group education sessions, have a check-off sheet that must be completed before they’re able to use the new sharps device in practice.
8. Ensure Healthcare Worker Safety With Sharps
Estimates indicate that nearly 385,000 healthcare workers are injured by accidental needlesticks every year in the U.S. To avoid this from happening at your organization, include education on the safe use of needles and other sharps during initial and annual staff training. In addition to needlestick prevention, staff should know what to do in the case of an accidental needlestick. Healthcare leaders can refer to occupational safety standards for navigating bloodborne pathogen exposure incidents in the clinical setting.
Tip: Develop a needlestick injury protocol to minimize risk of incidences and maximize awareness around how to properly handle an injury, should one occur.
Learn More Ways to Promote Patient Safety
So, what are standard precautions in healthcare? Now that you understand what standard precautions include, you’ll be better prepared to improve safety for staff and patients alike. Continue to build on those safety efforts with IntelyCare’s latest facility guides and recommendations, optimizing outcomes for all.