Credentialing Process for Providers: Step-by-Step Guide

As a facility leader, hiring qualified staff is essential for meeting standards of care and building trust with your patients. But beyond vetting candidates through standard job applications and interviews, facilities must also take measures to complete the credentialing process for providers. This entails verifying a provider’s professional and educational background to ensure that they can practice competently.
Credentialing is crucial for maintaining professional integrity and protecting patient safety. In this article, we’ll outline three key steps for carrying out this process and answer frequently asked questions to give you a clearer overview of what it entails.
What Is Credentialing?
Provider credentialing is a process in which facilities and other types of healthcare organizations verify a provider’s background, licenses, and certifications to ensure they’re properly trained to care for patients. This is typically done as soon as a provider is hired and begins the onboarding process. While this process is also commonly referred to as physician credentialing or medical credentialing, all types of allied healthcare professionals — including nurses and social workers — should be verified by a facility upon hire.
Why Is Provider Credentialing Important?
Credentialing is crucial for ensuring that healthcare providers are qualified to deliver safe care and helps protect both facilities and patients from malpractice. Facilities participating in Medicare and Medicaid programs are also federally mandated to complete the medical credentialing process for providers — and failing to do so can result in loss of funding. Even if your facility doesn’t participate in these programs, other professional organizations like the Joint Commission also mandate credentialing in their accreditation standards.
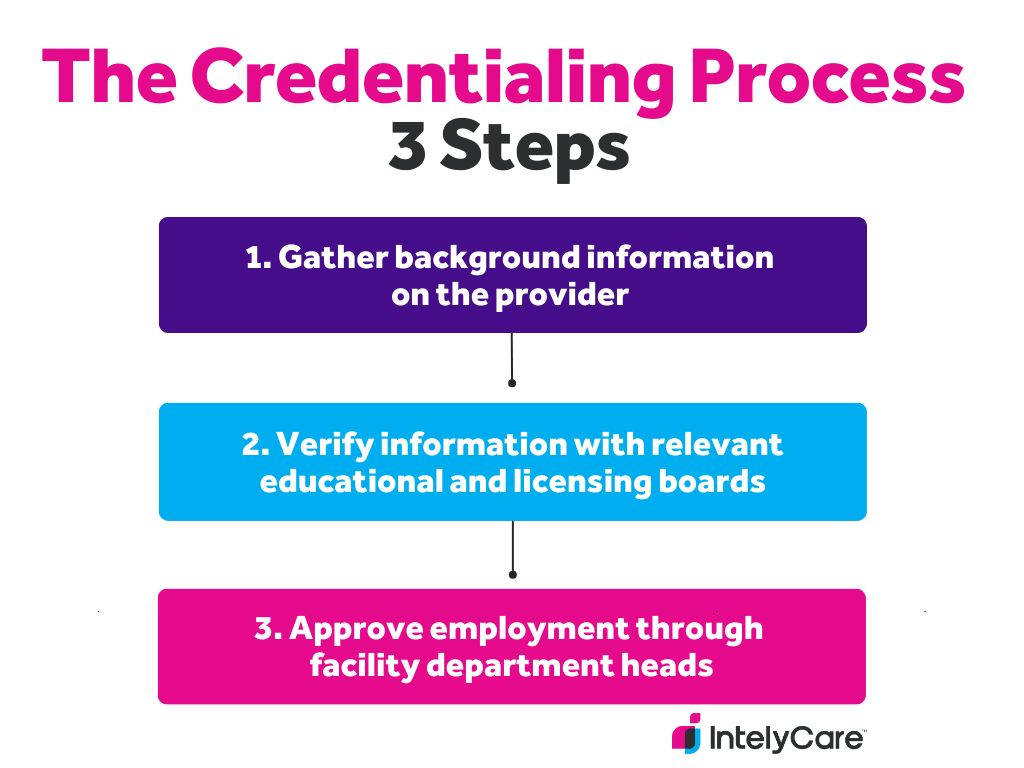
The Credentialing Process for Providers: 3 Steps
Now that you understand what credentialing is and why it’s important, you’re probably wondering how best to conduct this process at your facility. While this will look slightly different from organization to organization, here are three fundamental steps that go into a professional provider credentialing process.
1. Gather Information
The first step in the credentialing process is gathering essential information and supporting documents from your hired providers. This typically involves asking providers about their:
- Education and training.
- Employment/malpractice history.
- Licensure and certifications.
Some facilities may choose to hire third-party medical credentialing services that help gather this information. These companies, known as credential verification organizations (CVO), can make the credentialing process more efficient.
Tip: Individual states may have specific requirements for how hospitals should be credentialing providers. For example, Illinois requires all hospitals to collect information outlined in Section 965. Make sure that you double check your department of health’s requirements. If you choose to collect any supplemental information, standardizing an online application will make the process easier for both you and your new hires.
2. Verify Information
After you gather the information, you’ll need to verify it. Many facilities will correspond directly with the organizations that awarded the provider their credentials, such as educational institutions or licensing boards. However, you can also ask a CVO to carry out these verifications as well.
Tip: Verification shouldn’t end with the onboarding process. It’s important to continuously monitor a provider’s information to ensure that their credentials remain valid. Consider using a credentialing management platform that automatically notifies you when staff credentials expire or need to be re-checked.
3. Approve Employment
Approving employment is the last step in the credentialing process for providers. Once a facility receives and verifies a provider’s information, the department head usually meets with facility board members to do a final review of all documents. If there are no outstanding issues, they will go ahead and appoint the provider as staff.
Tip:Create a credentialing checklist that department heads and board members can use to review a provider’s information. This will ensure that all essential documents are accounted for, while helping to prevent errors.
Provider Credentialing FAQ
What is checked during a credentialing process?
The credentialing process in healthcare can vary depending on the state and facility a provider is hired to work in. Here are some examples of the types of information that facilities should verify:
- Education, training, and board certification eligibility
- Continuing education credits
- Work and employment history
- Clinical privilege history
- Names and emails of professional references
- Clinical performance reviews
- Malpractice insurance carriers and claims history
- Explanations for any gaps in education, training, or work history
- Federal, state, and professional licenses and registrations
What do credentialing companies do for providers?
Third-party credentialing companies work with providers to help them gather all the information and documents needed to complete the credentialing process. They also help facilities comply with federal regulations and complete verification checks with schools and licensing boards.
What is a credentialing fee?
A credentialing fee includes all the costs associated with completing the credentialing process. These fees are usually related to the time and resources needed to centralize applications, conduct background checks, and consult with educational/licensing boards.
Total fees for each provider usually range between $100 and $200. However, these fees can vary depending on how a facility’s credentialing system is set up and whether they’re using services from a CVO.
How long is the credentialing process for providers?
Credentialing in healthcare can take weeks to months, depending on several different factors. The process can take longer if facilities don’t have an efficient system for gathering and reviewing information, or if a provider delays sending over required documents.
Hire Providers Who Make the Credentialing Process Easy
Now that you understand the credentialing process for providers, you’ll want to find high quality candidates who can breeze through the verification stage of hiring. Reach over 1 million healthcare professionals who are actively seeking work on IntelyCare.