Technology in Nursing: 5 Ways Today’s Practice Is Affected
You are running behind on your med pass, two patients’ call lights are on, and a patient down in the radiology department is having a panic attack. You use your headset to ask your charge nurse for help and message the virtual nurse on EPIC to check on your patients who have their call lights on. You are now free to assess your patient in radiology.
How are you caring for all of your patients while they’re in different locations? That is the beauty of technology in nursing. Such advances have truly transformed the nursing profession. Some of the tasks nurses used to perform have been reduced by technology, allowing them to focus on other duties, such as improving patient care. Technology has also added more tasks, including training nurses on new devices or educating patients on their use.
The future of care will put more and more resources into digital advances that seek to deliver improved patient outcomes. Healthcare Information and Management Systems Society (HIMSS) led a study of healthcare stakeholders — including 359 clinicians and 1,600 patients — in Australia, Germany, New Zealand, the United Kingdom, and the United States. When asked whether it’s pivotal that their organizations make investments in digital technologies, 99% of health systems leaders in the U.S. and 95% of their international peers replied affirmatively.
Technology advances are ongoing and can change rapidly. We’ll discuss the current landscape of nursing and technology, the benefits of technology in nursing, and the impact of technology in nursing.
What Is Technology Used for in Nursing?
Technology is used in many different ways to help nurses perform their jobs more effectively, from easily accessing a patient’s medical history to providing patients with health information and beyond. Common examples include:
- Digital patient monitors (i.e., in-room vital sign monitor)
- Patient mobility lifts
- Smart beds
- Headsets, earpieces, and wearable badges for communication
- Medication scanners
- Electronic medical records (EMR)
- Electronic health records (EHR)
- Virtual simulations for education and training
- IV pumps
- Medication and supply Pyxis machines
- Defibrillators
- Telemetry monitoring systems
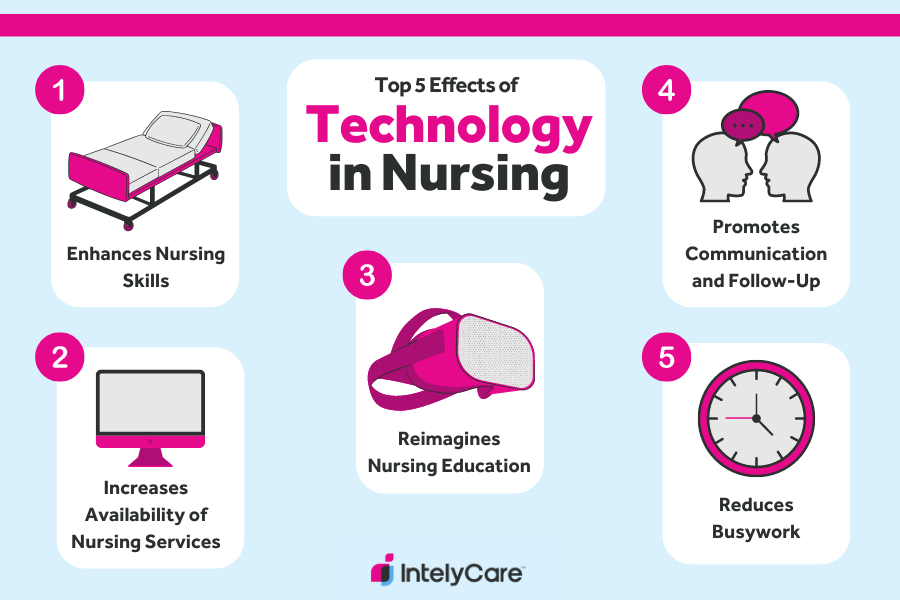
New Technology in Nursing: 5 Effects on Nursing Practice
All of the advances in medical technology are meant to improve a provider’s ability to deliver safe, high-quality patient care. For example, certain devices can help reduce medical errors, such as a medication scanner. If the nurse scans the wrong medication, the computer will alert the nurse of this discrepancy, prompting the nurse to double (or triple) check that medication before administering it. This is a huge — and potentially life-saving — benefit. Take a look at five other impacts technology is having on nursing.
1. Enhances Nursing Skills
One of the most important ways technology has impacted nursing practice is by enhancing and complementing nursing skills. Technology can aid nurses and other medical professionals with medication administration (i.e. automated IV pumps), obtaining vital signs (i.e. automatic blood pressure cuff), and patient mobility (i.e. electric patient lifts).
Example: View Finder
Consider a view finder (i.e., AccuVein), which is a common technology used in hospitals. As the name implies, this device allows nurses to observe veins for IV insertion using near-infrared visualization.
This device augments site selection and is extremely helpful on patients whose veins are not easily palpable, such as those with edema or dehydration. It can also make an IV insertion more likely to be successful, leading to less sticks for the patient.
Example: Smart Bed
Take the smart bed. Need to administer a dose of medication that’s dependent on a bedridden patient’s weight? No problem. Certain smart beds can calculate the correct dosage by weighing the patient to within the nearest 200 grams. The patient can be left undisturbed, and the nurses don’t need to exert excess energy repositioning a patient.
Speaking of, did you know that back pain is among the most common complaints among nursing professionals? No need to strain a nurse’s back muscles and spine when a smart bed can tilt laterally and allow for a much easier way to turn an immobile patient.
Example: RotoBeds
RotoBeds can be used to place ventilated patients in a prone position to improve outcomes for those with acute respiratory distress syndrome (ARDS) and severe COVID-19 infection. Without a bed to help, positioning a prone, sedated patient is labor intensive and requires a coordinated effort by a team of staff. Patient and staff safety are often put in jeopardy while completing these risky turns.
2. Increases Accessibility of Nursing Services
With the advent of telemedicine and virtual nursing, patients can visit with a nurse from the comfort of their own home. This helps save patients time and money and is especially beneficial to those with mobility issues, who lack easy access to transportation, and people living in rural areas.
Virtual nurses can also care for patients who are admitted to the hospital without being in the same physical location as the patient. How do they do this in real time? Through a camera on top of the TV in the patient’s room, like a video call.
These nurses can gather admission histories, monitor patients, perform safety rounds, implement pain assessments, provide patient education, complete MRI or preoperative checklists, write care plans, and even sign off as a witness for another nurse administering medication. This not only improves staffing, but it also allows nurses more flexibility over their work environment.
3. Reimagines Nursing Education
Did you know that technology in nursing benefits education too? Consider nursing school lab simulations that have mannequins capable of mimicking real-life medical scenarios.
Example: Clinical Simulations and Virtual Reality
For example, nursing instructors can control mannequin settings and replicate a specific clinical presentation for teaching purposes. They can then read off a case study and have the nursing student interact with the simulation mannequin, such as auscultating lung sounds and heart tones or even practicing inserting an IV.
Virtual reality (VR) environments are the next generation of clinical simulations, using a headset and hand controllers to create an immersive student experience. An instructor facilitates the experience in real time, using interactive software. Although this style of simulation lacks the hands-on experiences that mannequins provide, the cost of buying and maintaining a VR system is considerably less — and they’re totally portable.
As virtual simulations, completed entirely online, became more sophisticated, they became more widely used by nursing programs. Students interact independently with virtual patient scenarios and often only debrief the experiences in person with faculty. As long as a computer is available, scenarios can be completed at any time, and any place, making them convenient for busy students.
Simulations allow for authentic interactive experiences for nursing students, further promoting their education and setting them up for success in their profession. Technology provides a great way to practice nursing skills and critical thinking in well-controlled, safe settings.
In addition, the time spent completing simulations can be used to replace student clinical hour requirements, depending on individual state guidelines. The National Council of State Boards of Nursing (NCSBN) recommends that up to 50% of traditional clinical hours can be replaced safely with high-quality simulation experiences. Students benefit from opportunities to develop their skills outside of high-stress hospital environments, and facilities are less overburdened by the demands of student groups.
4. Promotes Communication and Follow-Up
Technological advances have enhanced communication amongst healthcare professionals and patients. For example, mobile apps paired with a patient’s EMR allow patients to engage in video conferencing with nurses or doctors, send messages and ask questions, and review labs and test results.
This also allows nurses to follow up with patients more closely and conveniently, as some patients may face barriers in keeping follow-up appointments. Also, nurses and other team members can communicate confidentially within the EMR while accessing a patient’s chart to avoid confusion over which patient they are discussing.
Example: Wearable Devices
In the clinical setting, wearable devices are used to keep in contact with nurses wherever they are on the unit. At the push of a button, a charge nurse can immediately reach a CNA to ask for patient assistance. The next generation of these wireless communication badges were voice-activated — nurses don’t have to stop what they’re doing or remove their gloves to use the device, making communication easier than ever. And to protect the nurse, many badges also have a panic button for emergencies.
Clinical decision support (CDS) systems are built into many EHR systems to enhance nurse decision-making and follow-up. For example, an alert can be triggered if a patient’s vital signs show a dangerous trend. When pre-established criteria are met, the EHR will fire an alert to notify the nurse and prompt them to take action. Recommendations can even be made based on facility policy.
CDS is an area of explosive growth with the advances brought by artificial intelligence (AI) and machine learning. By incorporating AI into CDS, recommendations can be made based on huge volumes of data that would be difficult — if not impossible — for a human to process. And AI can complete these computations in seconds. However, oversight of AI and the ethics of its use are hot topics for discussion.
5. Reduces Busywork
Arguably, one of the coolest technological advances in nursing is delivery robots. They can deliver meals, take medical specimens to the lab, bring linens to a patient’s room, and even fetch medications from the pharmacy. These are tasks that involve many, many steps but very little nursing expertise.
If you think this is minuscule, consider that the average nurse walks four to five miles per shift. With new technology, nurses can spend more time on patient care since they do not have to walk all over the hospital or unit.
Example: Documentation Reduction
In addition, well-designed EHR systems help to reduce redundant and unnecessary documentation. Oftentimes, this requires the skill and expertise of a strong nursing informatics team to customize content to match the facility’s policies and nursing workflows. The EHR should make documentation more streamlined for nurses, instead of adding work or making things more difficult.
Making sure systems and devices are interoperable, or able to “speak” to each other, is crucial for reducing busywork. For example, vital signs from the monitor should ideally be carried over automatically to the EHR, where the nurse only needs to review and verify the data instead of entering it from scratch. IV pumps should also connect with the EHR to make care more efficient and safe.
Common Challenges Nurses Face With Technology
For all of the advantages, never forget that technology can and does fail. When technology is involved in patient care, malfunctions can cause an inconvenience, delay, error, or patient harm. To mitigate errors and patient harm, it’s important for nurses to avoid operating on autopilot or putting all their trust in technology.
Nurses must also be aware of cybersecurity risks when using digital devices. As healthcare organizations become more reliant on technology, the need to ensure patient data security also grows. Data breaches and cyberattacks are increasing across the healthcare industry. As frontline workers, nurses have to be on the lookout for suspicious behaviors and security risks.
Furthermore, new technological advances can often bring additional roles and responsibilities for nurses. There’s nothing wrong with learning new things — but sometimes new things add to the nurse’s already full workload.
Some EMRs give patients access to portions of their medical charts on their phone or computer, with programs like MyChart. This means that the nurse has a new role of screening for digital literacy and teaching patients how to access and use MyChart.
Some patients may not know how to use a computer or smartphone, lack access to these technologies, live in an area without cell-service, or be unable to pay for internet services. Nurses need to screen for these barriers and connect patients to the appropriate resources, which can add to their already full plates.
Common technology challenges nurses face include:
- Broken or malfunctioning equipment
- Lacking uniformity (i.e., IV pumps vary from facility to facility)
- Electronic medical record (EMR) downtime
- Computer or device freezing
- Dead battery
- Devices unavailable during updates
- Limited training
- Disrupted workflows
- Change fatigue (too many new technologies)
- Varying comfort levels using technology
How Will Technology Change Nursing in the Future?
The growing presence of AI likely poses many questions around nursing and technology. Will nurses be replaced? Will hospitals be run by robots? Will everything become simulated and virtual?
While it’s a valid concern to wonder how the nursing profession will change in the future, it’s unlikely that technology will replace nurses. There’s nothing that can replace the human connection and experience that nurses bring to the table.
Imagine a family whose lives suddenly changed after a loved one received an unexpected diagnosis. No robot can match the comfort and support that an empathetic nurse provides.
Furthermore, an overreliance on technology isn’t recommended. If nurses are observing a patient’s symptoms that are contrary to the information that’s being displayed on a screen, those nurses will rely on what they’re seeing with their own eyes and act accordingly.
Software and technology may continue to supplement the nursing practice by reducing errors, saving time, increasing accessibility, allowing nurses to see more patients, and promoting communication.
How Will You Use Technology in Nursing?
One underrated perk of technology in nursing is the amazing ability to select your work from your phone, with jobs from IntelyCare. Apply for a nursing role that fits your life today.
Kerry Larkey, MSN, RN, contributed to the writing of this article.





