A Guide to Cultural Competence in the Care of LGBTQ Patients

Nearly 8% of U.S. adults identify as lesbian, gay, bisexual, transgender, or queer/questioning (LGBTQ), including an estimated 1.6 million transgender individuals. Despite strides towards equality, LGBTQ patients still face significant disparities in healthcare access and quality, often delaying or skipping care due to discrimination. Transgender individuals, in particular, face high rates of mistreatment and denial of care, highlighting the need for improved cultural competence in the care of LGBTQ patients in healthcare settings.
In this article, we’ll explore the ins and outs of culturally competent care for LGBTQ patients that promotes respect, sensitivity, and equity.
Cultural Competence in the Care of LGBTQ Patients: Key Facts
Navigating healthcare with cultural sensitivity is vital, especially when it comes to caring for LGBTQ patients. It’s about customizing care to match each person’s needs, so they feel heard, respected, and supported. But how can nurses practice culturally congruent care effectively? Here are a few things to keep in mind:
- LGBTQ communities are diverse, including lesbian, gay, nonbinary, and bisexual individuals, among others. Each person brings their own experiences, challenges, and healthcare needs.
- LGBTQ patients face health disparities compared to their heterosexual and cisgender counterparts. Discrimination, stigma, limited access to quality healthcare, and social factors all play a part in this.
- LGBTQ patients have unique healthcare needs. Transgender individuals, for example, may require gender-affirming care, hormone therapy, and gender-confirmation surgeries.
- LGBTQ care begins with organizational policies. It’s crucial to advocate for inclusive policies at healthcare organizations, which means training staff on LGBTQ cultural competency, using inclusive language and forms, and offering gender-neutral facilities.
- LGBTQ patients have rights. To be a good advocate, make sure you know about anti-discrimination laws, patient privacy, and the resources available to support your patients throughout their healthcare experience.
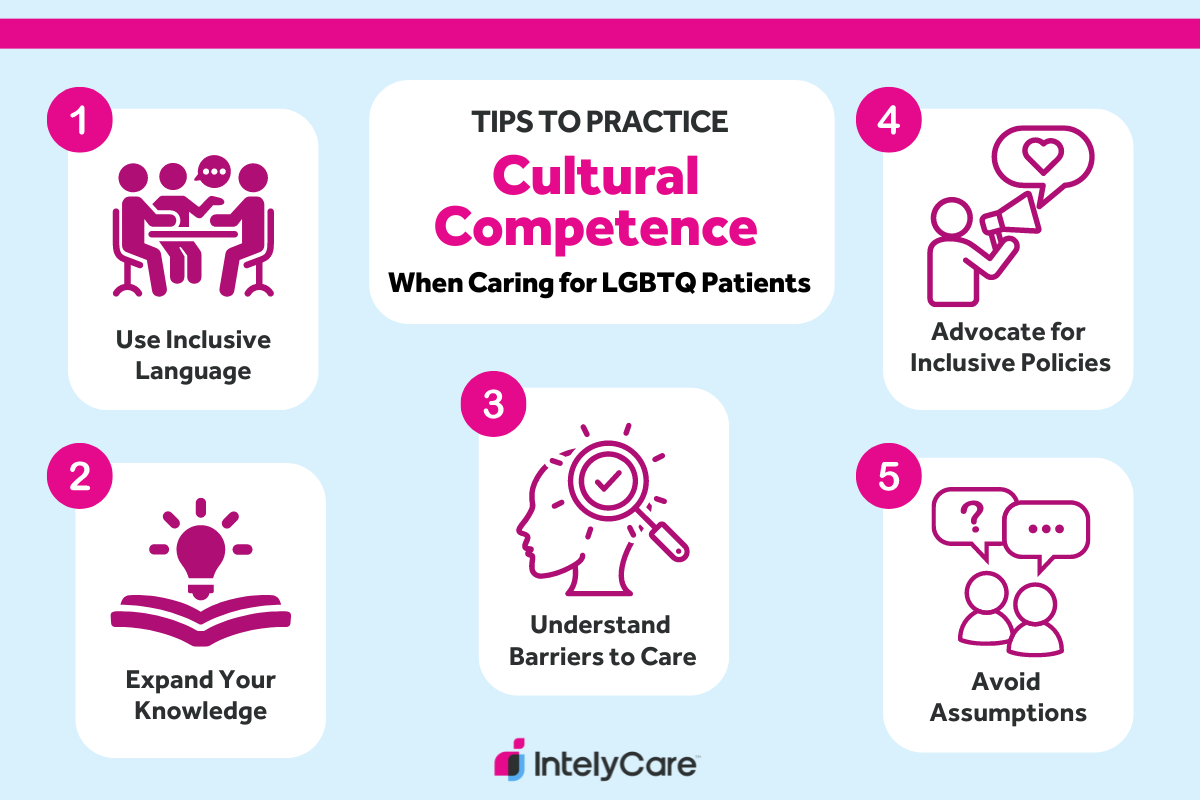
5 Tips for Practicing Cultural Competence in the Care of LGBTQ Patients
- Use inclusive language.
- Expand your knowledge.
- Understand barriers to care for LGBTQ people.
- Advocate for inclusive healthcare policies.
- Avoid assumptions.
1. Use Inclusive Language
How should you refer to an LGBTQ patient? Start by avoiding assumptions about patients’ gender identity or sexual orientation and using gender-neutral terms whenever possible. Here are some examples:
- Use words like “partner” or “spouse” instead of “husband” or “wife.”
- Use the word “they” instead of “he” or “she” until the patient has specified their preference.
- Ask open-ended questions whenever possible. Instead of asking “Are you straight or gay?” ask “How do you describe your sexual orientation?”
- Use the language the patient prefers. For example, if your patient states they are “female,” avoid calling them “transgender,” even if you know that information from their medical history. Refer to your patient as “female.”
- Don’t assume sexual orientation based on gender. You might have a patient who is a transgender female who would identify as lesbian or straight.
2. Expand Your Knowledge
LGBTQ education for healthcare providers sets the foundation for inclusive and supportive patient care. While some healthcare organizations offer LGBTQ cultural competency training to help staff better understand and address the needs of LGBTQ individuals, there is also a variety of free resources to help you build cultural competency. Here are some options:
- Attend online courses and workshops.
- Complete continuing education programs.
- Study relevant information on government websites, such as the National Coalition for LGBTQ Health.
- Read open-access journals, such as LGBT Health.
3. Understand Barriers to Care for LGBTQ People
Discrimination and stigma within healthcare settings can create significant barriers to accessing culturally competent care for LGBTQ patients. Nurses can help break down these barriers and support LGBTQ patients in accessing care. Common barriers include:
- Discrimination: Healthcare providers may hold personal biases or prejudices against LGBTQ individuals, affecting the quality of care.
- Fear of disclosure: Concerns about confidentiality may prevent LGBTQ individuals from disclosing their sexual orientation or gender identity to healthcare providers.
- Limited access to gender-affirming care: Transgender individuals may struggle to access hormone therapy or gender-confirmation surgery.
- Geographic barriers: LGBTQ individuals living in remote or rural areas may have limited access to healthcare services that are LGBTQ-friendly.
- Lack of support: Some LGBTQ individuals may face rejection by families and lack familial support in navigating the healthcare system.
- Mental health stigma: Stigma surrounding sexual orientation or gender identity can negatively impact the mental health of LGBTQ individuals.
4. Advocate for Inclusive Healthcare Policies
Nurses are frontline advocates for cultural competence in the care of LGBTQ patients, striving to create healthcare environments where all patients feel supported and valued. To promote inclusive policies, nurses can:
- Join professional nursing associations or LGBTQ advocacy groups.
- Advocate for the implementation of LGBTQ cultural competency training programs for healthcare staff.
- Promote the use of gender-affirming language in healthcare settings.
- Collaborate with LGBTQ healthcare organizations to identify and address healthcare disparities.
- Educate colleagues and healthcare administrators about the importance of LGBTQ-inclusive policies.
- Stay informed about current legislative efforts and policy changes related to LGBTQ healthcare rights at local, state, and national levels.
5. Avoid Assumptions
Caring for LGBTQ patients isn’t one-size-fits-all — you must tailor care to each person’s unique needs. Each person within each subgroup of the LGBTQ community has unique treatment goals. For example, a transgender patient may require access to hormone therapy and gender confirmation surgeries to align their body with their gender identity. Other community members may have specific sexual health needs, such as HIV prevention and screening.
While common treatment goals may exist, it’s important to avoid assumptions. For instance, not all individuals who identify as transgender may seek hormone therapy. Additionally, just because someone is a member of the LGBTQ community doesn’t mean they seek HIV prevention education. In fact, these assumptions can be hurtful to your patient. Instead, listen to your patients, ask open-ended questions, and tailor care to their needs.
Cultural Competence in the Care of LGBTQ Patients: FAQs
How do you address an LGBTQ patient?
To address an LGBTQ patient, it’s important to use inclusive language that respects their gender identity and sexual orientation. Start by asking the patient their preferred name and pronouns, and use them consistently throughout the interaction.
What are some common misconceptions about LGBTQ patients in healthcare?
Common misconceptions about LGBTQ patients include assuming all gay men are at high risk for HIV, or that all trans patients are seeking gender-affirming surgery. Additionally, there may be stereotypes that LGBTQ individuals are more prone to mental health issues solely because of their sexual orientation or gender identity. Healthcare providers must recognize and challenge these misconceptions to ensure respectful care for all patients.
What healthcare needs might a transgender patient have?
In addition to routine medical care, including preventive screenings and vaccinations, the types of healthcare services that an individual transgender patient might seek in healthcare facilities may include:
- Hormone replacement therapy (HRT)
- Surgical procedures to modify primary and/or secondary sexual characteristics
- Counseling or therapy to address gender dysphoria and other mental health concerns
- Gynecological and reproductive health services
- Sexual health screenings and education
- Gender-affirming voice therapy
- Legal and social services to make changes on identification documents
What are some helpful resources for LGBTQ patients?
Helpful resources for LGBTQ patients in the U.S. healthcare system include LGBTQ-affirming healthcare providers listed in directories like the LGBTQ Healthcare Directory. Patients can also use online resources like the Human Rights Campaign’s Healthcare Equality Index to find facilities prioritizing LGBTQ-inclusive care.
Ready to Find a New Nursing Job?
Ready to put your knowledge of cultural competence in the care of LGBTQ patients into action in your new role? IntelyCare offers job matching for nursing professionals to help you find the best-fitting roles — in the right specialty, facility, and location.
