What Is Person-Centered Care? Overview and FAQ

Person-centered care refers to an approach that prioritizes a patient’s individual needs, preferences, and values. Medical protocols guide healthcare providers in diagnosing and treating various types of health conditions. By following best practices, providers work toward achieving the best possible patient outcomes. But what happens when they deviate from condition-based care and start considering a patient’s bigger life picture? Lives change.
In this article, we cover what it means to provide person-focused care at your healthcare facility, answer frequently asked questions about this approach, and explore realistic care examples across different healthcare settings.
What Is Person-Centered Care?
Person-centered care is a way to strengthen the provider-patient relationship by emphasizing patient engagement and shared decision-making. This care approach encourages patients to actively participate in their care, set health goals, and collaborate with their healthcare team to achieve better outcomes over time.
Delivering care that is person-centered can improve patient satisfaction, treatment outcomes, and the overall quality of care. It can be applied in healthcare settings such as:
- Hospitals
- Ambulatory care centers
- Primary care clinics
- Long-term care facilities
- Mental health treatment centers
Person-Centered vs. Patient-Centered Care: What’s the Difference?
While both person- and patient-centered care focus on recognizing what a patient’s problems are beyond their diagnosis, these care approaches have some fundamental differences. Person-focused care is about building long-term relationships, while patient-centered care is more focused on episode-based treatment. The table below outlines some of the more specific differences between these two care approaches.
| Person-Centered Care | Patient-Centered Care |
|---|---|
| Focuses on relationship-building over time
Considers each episode of treatment in context to the larger life-course experience Considers how all diseases might be related Views body systems as interrelated More focus on people’s experiences with general health as well as their diseases Uses coding systems that are adaptable to people’s specific health concerns |
Focuses on interactions during each visit
More episode-oriented Centers around disease management Views body systems as distinct More focus on the evolution and prognosis of a patient’s disease Uses coding systems build off of professionally-defined conditions |
What Is Included in the Patient-Focused Care Model?
A person-focused care model takes a comprehensive, whole-person approach when addressing an individual’s well-being. It recognizes that a person’s health is influenced by their socioeconomic status, education, access to care, living situation, and community — or the factors known as the social determinants of health. By addressing and recognizing the social determinants, healthcare providers can deliver comprehensive care that improves overall well-being and health outcomes for individuals.
The Centers for Medicare and Medicaid Services (CMS) recommends integrating this approach as part of a value-based care model. According to CMS, the following components should be included when integrating person-focused care at your healthcare facility.
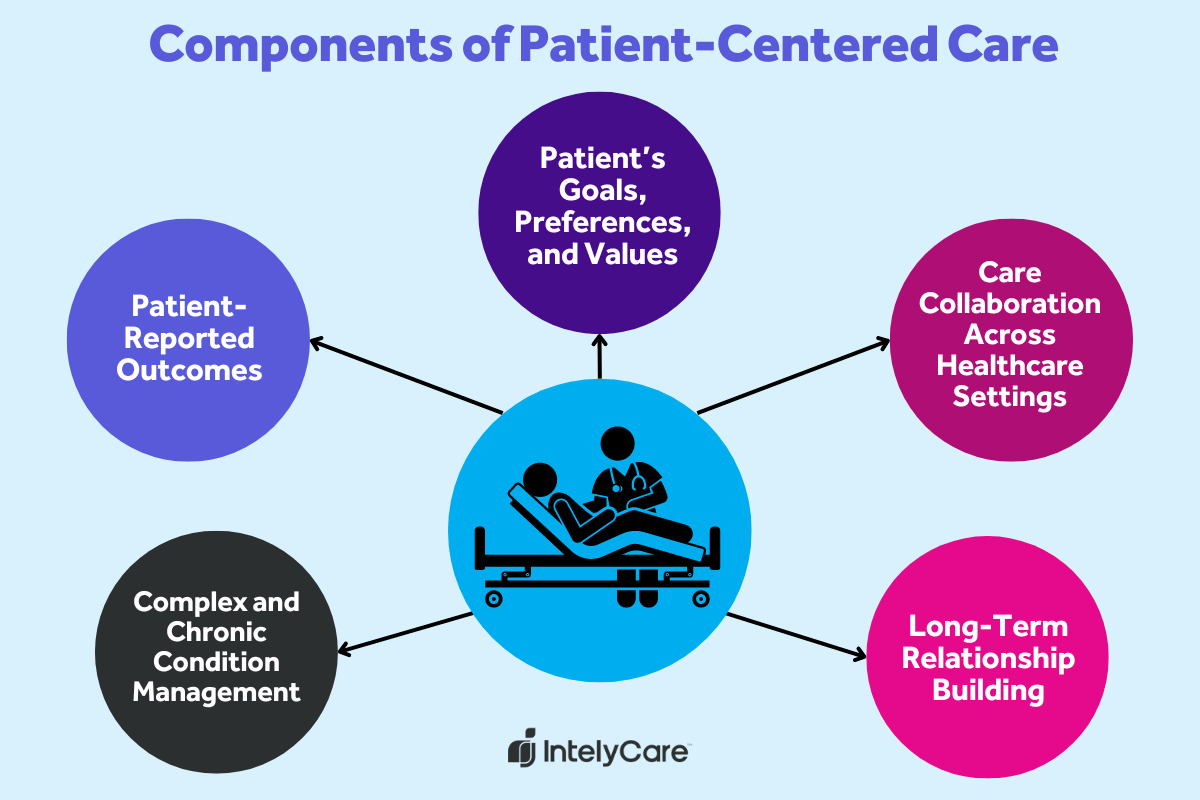
1. Patients’ Goals, Preferences, and Values
Healthcare providers collaborate with patients by considering the personal preferences and emotional factors that contribute to their well-being. Patients are viewed as active participants in their care who have a right to make informed health decisions. By prioritizing autonomy, providers build a trusting and empowered relationship with patients.
Example: An older adult sees an oncologist for a new cancer diagnosis. The patient shares his goals for the near future, which include attending his daughter’s wedding. Together, he and the oncologist select a treatment plan that allows him to maximize his quality of life so he can walk his daughter down the aisle.
2. Patient-Reported Outcomes
In conventional medicine, objective data like vital signs and lab values help healthcare providers measure an individual’s response to medical treatment. With person-focused care, patient-reported outcomes are taken into account as well. This concept encourages patients to actively participate in their care and create goals for their individualized care plan.
Example: A patient with chronic liver disease discusses ongoing depression with their primary provider. The provider creates a “homework assignment” for mood-boosting activities to work on between appointments. At the next appointment, the patient evaluates their depression symptoms using a self-reporting questionnaire.
3. Care Collaboration Across Healthcare Settings
Person-centered care creates a culture of safety by integrating care across healthcare settings. It allows providers to access patient information to provide individualized care — and avoid errors during care transitions. It also allows caregivers to collaborate about a patient’s individual preferences, such as religious or cultural practices.
Example: A patient is directly admitted to the hospital for surgery from a primary care office. The primary care nurse practitioner places information in the chart about the patient’s decision to refuse blood products. The hospital team honors this request when accepting the patient for surgery.
4. Complex and Chronic Condition Management
Patients with complex and chronic diseases often see multiple healthcare providers in their lifetime. Person-focused care allows providers to collaborate across specialties while keeping the main focus on the patient’s holistic well-being.
Example: A patient with a history of diabetes, obesity, and kidney failure is hospitalized for a hypertensive crisis. A member of the nursing staff, who knows the patient well, requests a low-sodium diet from the kitchen and places signage throughout the room to avoid blood pressures and venipuncture in the left arm due to the presence of a dialysis fistula.
5. Long-Term Relationship Building
One of the key goals of person-focused care is to establish trusting long-term relationships between patients and providers. To be successful, providers must be flexible and adapt to a person’s changing needs or preferences over time. Providers encourage feedback so they can continuously improve patient care. It also considers emerging issues for older adults, such as creating a care plan that includes their caregiver in decision-making.
Example: An older adult is the primary caregiver for their parent with advanced dementia. At a primary care appointment, the provider creates a care plan that includes respite care and other resources for the family caregiver.
Seeking More Tips on Best Practice Care?
Part of a commitment to quality healthcare care is the integration of person-centered care in nursing and advanced practice environments. Learn more ways to promote best practice care when you sign up for IntelyCare’s monthly newsletter.





